Humble Hookworms – Your Friend or Foe?
 Research being undertaken right here in Canterbury and supported by the Gut Foundation is finding the answer to this question
The thought of having hookworms in your intestines may be difficult for some people to swallow but a new collaborative study performed between researchers in Christchurch and Australia asked people with coeliac disease to do just that. Research funded by the Bowel and Liver Trust has previously showed high rates of coeliac disease in Canterbury with 1/84 Cantabrians being affected. The disease is caused by an immune reaction to gluten (a protein found in wheat, barley, oats and rye), which leads to permanent damage to the lining of the small intestine due to inflammation. This damage reduces the surface area of the small intestine, leading to reduced absorption of nutrients and gastrointestinal symptoms. The treatment of coeliac disease is almost always successful but requires patients to remove all gluten containing foods from the diet. This can lead to a significant reduction in quality of life for people who are affected.
it seems that these parasitic worms produce molecules beneficial to gut flora in people suffering from inflammatory diseases of the digestive tract. It’s called worm-induced immune modulation and, it could be a global game-changer.
Professor Richard Gearry is a leading gastroenterologist based in Christchurch and has been instrumental in the trans-Tasman collaboration, both clinically, and as a member of the Gut Foundation.
He says a recent open-label proof-of-principle clinical trial in Melbourne showed infections with low numbers of Hookworms were safe and enabled people with Coeliac Disease to tolerate eating a medium sized bowl of pasta with no ill-effects.
That’s an incredible finding. The established protocol for managing Coeliac Disease is a gluten-free diet. But it doesn’t always alleviate the symptoms, plus it is expensive, inconvenient, and inadvertent gluten exposure is common.
For trial participants, the thought of a bowl of pasta without the health repercussions was enough to tolerate the deliberate infection of Hookworms.
The next step is to identify the molecules that induce immunomodulation with a view to developing a medication. Larger placebo-controlled clinical trials are required and the Bowel and Liver Trust is committed to fundraising to support this ground-breaking research
Did you know?
Research being undertaken right here in Canterbury and supported by the Gut Foundation is finding the answer to this question
The thought of having hookworms in your intestines may be difficult for some people to swallow but a new collaborative study performed between researchers in Christchurch and Australia asked people with coeliac disease to do just that. Research funded by the Bowel and Liver Trust has previously showed high rates of coeliac disease in Canterbury with 1/84 Cantabrians being affected. The disease is caused by an immune reaction to gluten (a protein found in wheat, barley, oats and rye), which leads to permanent damage to the lining of the small intestine due to inflammation. This damage reduces the surface area of the small intestine, leading to reduced absorption of nutrients and gastrointestinal symptoms. The treatment of coeliac disease is almost always successful but requires patients to remove all gluten containing foods from the diet. This can lead to a significant reduction in quality of life for people who are affected.
it seems that these parasitic worms produce molecules beneficial to gut flora in people suffering from inflammatory diseases of the digestive tract. It’s called worm-induced immune modulation and, it could be a global game-changer.
Professor Richard Gearry is a leading gastroenterologist based in Christchurch and has been instrumental in the trans-Tasman collaboration, both clinically, and as a member of the Gut Foundation.
He says a recent open-label proof-of-principle clinical trial in Melbourne showed infections with low numbers of Hookworms were safe and enabled people with Coeliac Disease to tolerate eating a medium sized bowl of pasta with no ill-effects.
That’s an incredible finding. The established protocol for managing Coeliac Disease is a gluten-free diet. But it doesn’t always alleviate the symptoms, plus it is expensive, inconvenient, and inadvertent gluten exposure is common.
For trial participants, the thought of a bowl of pasta without the health repercussions was enough to tolerate the deliberate infection of Hookworms.
The next step is to identify the molecules that induce immunomodulation with a view to developing a medication. Larger placebo-controlled clinical trials are required and the Bowel and Liver Trust is committed to fundraising to support this ground-breaking research
Did you know?
- 1 in 80 New Zealanders have Coeliac’s Disease.
- New Zealand has one of the highest rates of inflammatory bowel disease (Crohn’s Disease/ulcerative colitis) in the world, mainly affecting people 15-35yrs.
- More than 3,500 people are diagnosed with bowel cancer every year in NZ.
- A 2014 research study showed the incidence of Inflammatory Bowel Disease (IBD) increased by 50% over a ten-year period in Canterbury alone.
Endoscopic Ultra sound for the south Island
 Imagine swallowing a pill that can take photographs of your intestine and send them wirelessly to a data recorder so that they can be downloaded, like a movie, for your doctor to review at a computer workstation.
While this may sound like the work of a science fiction novelist, it became a reality in 2002 when The Bowel and Liver Trust raised money for the first capsule endoscopy system available in a public hospital in New Zealand. This work was driven by then Chair of the Bowel and Liver Trust, Mr Martin Howman, who led a team of Trustees to raise the money to provide this important service to Cantabrians.
In the 1970s flexible gastroscopes and colonoscopes had been introduced to examine the stomach and colon, respectively. However, the small intestine, which is between the stomach and colon, has always been difficult to visualise and diagnose diseases in. The advent of Pillcam has changed the way that doctors view the small intestine - the final frontier of gastroenterology. Now patients can undergo a non-invasive test without being admitted to hospital.
The Pillcam was the brainchild of an unlikely combination – an Israeli Astrophysicist and an American Gastroenterologist. Each capsule (the size of a large pill) contains a small camera, a light, a battery and a transmitter. The light flashes twice per second with a photo taken each time. The images are sent wirelessly to a data recorder,
which is worn as a belt around the waist.
As Dale Cornelius, Capsule Nurse, explains, “the patient simply swallows a Pillcam capsule in the morning after an overnight fast. The data recorder is fitted to the patient who can then go about their usual activities for the day before returning to the clinic where the data recorder is removed and the images are downloaded to a computer. Software in the computer converts the images into a video, which can be analysed by a gastroenterologist. Each study takes between 30 and 60 minutes to analyse and report.” Dale Cornelius is currently undergoing training to
assist in interpretation of the studies.
Improvements in technology have led to longer battery life with 10 hours now allowing for the entire small intestine to be easily examined. The angle of the lens has also increased allowing more of the intestine to be examined with
each picture. It is hoped that improvements in software may improve the identification of abnormalities.
Dr Bruce Chapman, Gastroenterologist and Trustee says that a frequently asked question by patients is, “are the capsules reused?” The answer, to the relief of the patient, is “no” with a new capsule being used for every patient. The Pillcam system can be used for all age groups including children and the elderly. Dale Cornelius recently performed a study in an 88-year patient who completed the study with ease.
The Pillcam is very helpful for identifying sources of bleeding in the small intestine, defining extent of
disease in small bowel Crohn’s disease. More rarely it is used to identify polyps and small intestinal tumours. In a review of local cases 59% of those referred with anaemia had a positive finding and in 77% of patients referred
with diarrhoea there was a positive finding.
Imagine swallowing a pill that can take photographs of your intestine and send them wirelessly to a data recorder so that they can be downloaded, like a movie, for your doctor to review at a computer workstation.
While this may sound like the work of a science fiction novelist, it became a reality in 2002 when The Bowel and Liver Trust raised money for the first capsule endoscopy system available in a public hospital in New Zealand. This work was driven by then Chair of the Bowel and Liver Trust, Mr Martin Howman, who led a team of Trustees to raise the money to provide this important service to Cantabrians.
In the 1970s flexible gastroscopes and colonoscopes had been introduced to examine the stomach and colon, respectively. However, the small intestine, which is between the stomach and colon, has always been difficult to visualise and diagnose diseases in. The advent of Pillcam has changed the way that doctors view the small intestine - the final frontier of gastroenterology. Now patients can undergo a non-invasive test without being admitted to hospital.
The Pillcam was the brainchild of an unlikely combination – an Israeli Astrophysicist and an American Gastroenterologist. Each capsule (the size of a large pill) contains a small camera, a light, a battery and a transmitter. The light flashes twice per second with a photo taken each time. The images are sent wirelessly to a data recorder,
which is worn as a belt around the waist.
As Dale Cornelius, Capsule Nurse, explains, “the patient simply swallows a Pillcam capsule in the morning after an overnight fast. The data recorder is fitted to the patient who can then go about their usual activities for the day before returning to the clinic where the data recorder is removed and the images are downloaded to a computer. Software in the computer converts the images into a video, which can be analysed by a gastroenterologist. Each study takes between 30 and 60 minutes to analyse and report.” Dale Cornelius is currently undergoing training to
assist in interpretation of the studies.
Improvements in technology have led to longer battery life with 10 hours now allowing for the entire small intestine to be easily examined. The angle of the lens has also increased allowing more of the intestine to be examined with
each picture. It is hoped that improvements in software may improve the identification of abnormalities.
Dr Bruce Chapman, Gastroenterologist and Trustee says that a frequently asked question by patients is, “are the capsules reused?” The answer, to the relief of the patient, is “no” with a new capsule being used for every patient. The Pillcam system can be used for all age groups including children and the elderly. Dale Cornelius recently performed a study in an 88-year patient who completed the study with ease.
The Pillcam is very helpful for identifying sources of bleeding in the small intestine, defining extent of
disease in small bowel Crohn’s disease. More rarely it is used to identify polyps and small intestinal tumours. In a review of local cases 59% of those referred with anaemia had a positive finding and in 77% of patients referred
with diarrhoea there was a positive finding.
 While some patients have requested a Pillcam instead of a colonoscopy, unfortunately this is currently not an option.
A Pillcam for the colon is under development and prototypes have been tested but there are limitations with the bowel preparation in the colon.
The Pillcam platform is available in Christchurch in both public and private health sectors and serves the upper half
of the South Island. About 100 capsule endoscopy studies are performed at Christchurch Hospital each year, with more than a thousand studies since the system was established in Canterbury in 2002.
Another great success for the Bowel and Liver Trust, improving the gastrointestinal health of New Zealanders.Read More...
While some patients have requested a Pillcam instead of a colonoscopy, unfortunately this is currently not an option.
A Pillcam for the colon is under development and prototypes have been tested but there are limitations with the bowel preparation in the colon.
The Pillcam platform is available in Christchurch in both public and private health sectors and serves the upper half
of the South Island. About 100 capsule endoscopy studies are performed at Christchurch Hospital each year, with more than a thousand studies since the system was established in Canterbury in 2002.
Another great success for the Bowel and Liver Trust, improving the gastrointestinal health of New Zealanders.Read More...Growing mini-guts to study bowel disease
 Aim
To develop a three dimensional cell structure that closely resembles the human gut as a means to model bowel disease.
Background
Our research is centred on understanding how bacteria-host interactions in the gut increase the risk of disease. We have shown that enterotoxigenic Bacteroides fragilis colonization of the human bowel occurs more often in patients with colorectal cancer than in healthy controls. Likewise, there is evidence that humans infected with Campylobacter jejuni may be at increased risk of developing Crohn’s disease. However, we do not yet fully understand the mechanisms that link carriage of these bacteria to increased risk of disease.
Single crypts or stem cells derived from the small intestine or colon can be expanded ex vivo over long periods to generate epithelial structures that closely resemble the self-renewing crypt-villus architecture of the gut. These organoids, which contain all differentiated types of cells and grow as three-dimensional structures, are essentially “mini-guts”. Accordingly, they potentially provide a model system of the respective niches that these (and other pathogens) colonize throughout the gastrointestinal tract to help us better understand specific host-pathogen interactions.
Research Design
We have ethical approval to grow mini-guts from mouse and human biopsies. The biopsies will be digested with EDTA and then fractionated to give a crypt-rich preparation that will be cultured on Matrigel in defined medium. Once the organoids become established, they will be maintained in a manner similar to that used for the ongoing culture of cell lines. The advantage of organoids over cell cultures is that the former will provide a near physiological ex vivo model of the gut that can be monitored in real time.
We propose to expose the organoids to bacteria and/or potential therapeutics to determine cell-specific host-pathogen responses. Specifically, we will use cell proliferation, markers of apoptosis and evidence of intestinal phosphatase activity to assess if an infection and/or therapeutic has a measurable effect of cell differentiation and therefore the rate of organoid growth. We will also extract RNA from the cells for quantitative analysis of those genes we are interested in. In addition, we will measure intestinal alkaline phosphatase activity in situ in organoid-derived cell homogenates as a measure of innate immunity.
Results/Outcomes
Aim
To develop a three dimensional cell structure that closely resembles the human gut as a means to model bowel disease.
Background
Our research is centred on understanding how bacteria-host interactions in the gut increase the risk of disease. We have shown that enterotoxigenic Bacteroides fragilis colonization of the human bowel occurs more often in patients with colorectal cancer than in healthy controls. Likewise, there is evidence that humans infected with Campylobacter jejuni may be at increased risk of developing Crohn’s disease. However, we do not yet fully understand the mechanisms that link carriage of these bacteria to increased risk of disease.
Single crypts or stem cells derived from the small intestine or colon can be expanded ex vivo over long periods to generate epithelial structures that closely resemble the self-renewing crypt-villus architecture of the gut. These organoids, which contain all differentiated types of cells and grow as three-dimensional structures, are essentially “mini-guts”. Accordingly, they potentially provide a model system of the respective niches that these (and other pathogens) colonize throughout the gastrointestinal tract to help us better understand specific host-pathogen interactions.
Research Design
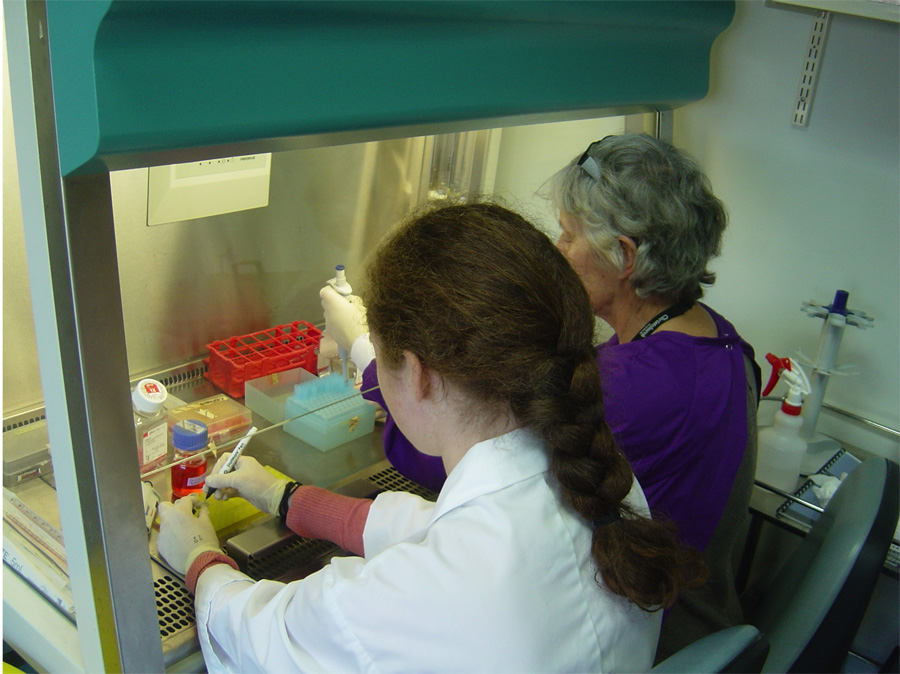
We have ethical approval to grow mini-guts from mouse and human biopsies. The biopsies will be digested with EDTA and then fractionated to give a crypt-rich preparation that will be cultured on Matrigel in defined medium. Once the organoids become established, they will be maintained in a manner similar to that used for the ongoing culture of cell lines. The advantage of organoids over cell cultures is that the former will provide a near physiological ex vivo model of the gut that can be monitored in real time.
We propose to expose the organoids to bacteria and/or potential therapeutics to determine cell-specific host-pathogen responses. Specifically, we will use cell proliferation, markers of apoptosis and evidence of intestinal phosphatase activity to assess if an infection and/or therapeutic has a measurable effect of cell differentiation and therefore the rate of organoid growth. We will also extract RNA from the cells for quantitative analysis of those genes we are interested in. In addition, we will measure intestinal alkaline phosphatase activity in situ in organoid-derived cell homogenates as a measure of innate immunity.
Results/Outcomes
- This model will be developed by Gabrielle Budd, mentored by Jacqui Keenan and Andrew Day. Gabby is a medical student who has been working over the summer on a studentship sponsored by the Bowel and Liver Trust. This project is a continuation of that research.
- It is envisaged that this research will provide us with a biologically relevant model to better understand the role of gut bacteria in the aetiology of inflammatory bowel disease and colorectal cancer. Accordingly, we propose to present our preliminary findings at local and national scientific meetings
- The pilot data we generate from this study will be used to support subsequent proposals to other funding agencies.
Summer studentships sponsored by the trust
 Student Gabrielle Budd
Title: Intestinal membrane vesicles – A novel innate defense mechanism?
Supervisor(s): Dr. Jacqui Keenan, Professor Andrew Day
Sponsor: Bowel and Liver Trust
Introduction: Crohn’s disease is a non-curable inflammatory condition of the intestinal tract. It is thought to be caused by an inappropriate and self-perpetuating reaction to intestinal bacteria. The severity of symptoms often fluctuates, with cycles of ‘flares’ and periods of remission. Treatment for most individuals involves high doses of drugs that suppress the immune system, but often these have significant side effects such as increased susceptibility to infection and hormone imbalances. Liquid diets are often used in children for this reason, and they have been shown to be as effective as corticosteroid drugs in inducing remission. Polymeric formula is one type of liquid diet used frequently for children with Crohn’s disease. The rationale for its use is that it reduces the work required to digest and absorb food, as well as being hypoallergenic and containing all the necessary components of a healthy diet. However, our research suggests that polymeric formula may also have additional effects on the innate immune response that include dampening the expression of inflammatory messengers and inhibition of bacterial binding to the surface of gut epithelial cells. It is currently unclear whether this effect of PF relates to direct antibacterial activity and/or an indirect effect. Indirect mechanisms include enhanced cell differentiation that is associated with increased production of membrane vesicles from the cell surface. These membrane vesicles have the potential to act as releasable decoys, thereby limiting bacterial binding to the intestinal epithelium.
Aims:
Student Gabrielle Budd
Title: Intestinal membrane vesicles – A novel innate defense mechanism?
Supervisor(s): Dr. Jacqui Keenan, Professor Andrew Day
Sponsor: Bowel and Liver Trust
Introduction: Crohn’s disease is a non-curable inflammatory condition of the intestinal tract. It is thought to be caused by an inappropriate and self-perpetuating reaction to intestinal bacteria. The severity of symptoms often fluctuates, with cycles of ‘flares’ and periods of remission. Treatment for most individuals involves high doses of drugs that suppress the immune system, but often these have significant side effects such as increased susceptibility to infection and hormone imbalances. Liquid diets are often used in children for this reason, and they have been shown to be as effective as corticosteroid drugs in inducing remission. Polymeric formula is one type of liquid diet used frequently for children with Crohn’s disease. The rationale for its use is that it reduces the work required to digest and absorb food, as well as being hypoallergenic and containing all the necessary components of a healthy diet. However, our research suggests that polymeric formula may also have additional effects on the innate immune response that include dampening the expression of inflammatory messengers and inhibition of bacterial binding to the surface of gut epithelial cells. It is currently unclear whether this effect of PF relates to direct antibacterial activity and/or an indirect effect. Indirect mechanisms include enhanced cell differentiation that is associated with increased production of membrane vesicles from the cell surface. These membrane vesicles have the potential to act as releasable decoys, thereby limiting bacterial binding to the intestinal epithelium.
Aims:
- To determine if polymeric formula has a direct effect on bacterial cell growth
- To investigate whether membrane vesicles limit bacterial binding to the gut wall.
Tom Currie Summer Studentship
 I’m Tom Currie a 5th year medical student. This summer I undertook a summer studentship with Mr. Tim Eglinton,
a colorectal surgeon at Christchurch Hospital and Senior Lecturer at the University of Otago, Christchurch. The
Studentship studied the impact of a modern medication on the treatment of perianal Crohn’s Disease.
Crohn’s disease is a form of inflammatory bowel disease (IBD) that can affect any part of the gut from the mouth
to the anus. It is over represented in Canterbury when compared to international rates. Approximately 1 in 3 of
these patients develops problems in and around the anus (bottom) including abscesses and fistulas (abnormal tracts
between the anus and the skin). Recently developed medicines known as anti-TNF-α antibodies have been used
with some success to treat these complications of IBD.
The aim of my studentship was to determine the outcomes of patients treated with these medicines in Canterbury since their introduction and in particular whether any particular patients were more likely to respond to these medicines than others.
Seventy-five patients qualified for the study and data was collected from patient notes. The main findings were that 73% responded to the anti-TNF-α therapy but only 20% healed completely. We couldn’t identify any definite factors predicting a successful outcome with this treatment. However, we did find that the patients that didn’t respond
to anti TNF-α therapy tended to have more severe disease and despite their drug therapy many of them still required frequent surgery.
Surgery for severe perianal Crohn’s disease can be major, debilitating and can require a permanent stoma. For this reason further research into optimising the current therapies in this disease is necessary.
This research will need to focus the optimal duration of therapy, its combination with other medical and surgical treatments and whether any blood or genetic markers will help predict response to these potent medicines.
On a personal note it was a great experience to undertake this research and I’m sure what I learned will hold me in good stead for research in the future. It was also highly beneficial to learn about a disease in depth that affects our community on such a significant scale. I would like to thank Warner and Patsy Mauger for their very generous
sponsorship through the Bowel and Liver Trust: this would not have been possible without their help.
Tom CurrieRead More...
I’m Tom Currie a 5th year medical student. This summer I undertook a summer studentship with Mr. Tim Eglinton,
a colorectal surgeon at Christchurch Hospital and Senior Lecturer at the University of Otago, Christchurch. The
Studentship studied the impact of a modern medication on the treatment of perianal Crohn’s Disease.
Crohn’s disease is a form of inflammatory bowel disease (IBD) that can affect any part of the gut from the mouth
to the anus. It is over represented in Canterbury when compared to international rates. Approximately 1 in 3 of
these patients develops problems in and around the anus (bottom) including abscesses and fistulas (abnormal tracts
between the anus and the skin). Recently developed medicines known as anti-TNF-α antibodies have been used
with some success to treat these complications of IBD.
The aim of my studentship was to determine the outcomes of patients treated with these medicines in Canterbury since their introduction and in particular whether any particular patients were more likely to respond to these medicines than others.
Seventy-five patients qualified for the study and data was collected from patient notes. The main findings were that 73% responded to the anti-TNF-α therapy but only 20% healed completely. We couldn’t identify any definite factors predicting a successful outcome with this treatment. However, we did find that the patients that didn’t respond
to anti TNF-α therapy tended to have more severe disease and despite their drug therapy many of them still required frequent surgery.
Surgery for severe perianal Crohn’s disease can be major, debilitating and can require a permanent stoma. For this reason further research into optimising the current therapies in this disease is necessary.
This research will need to focus the optimal duration of therapy, its combination with other medical and surgical treatments and whether any blood or genetic markers will help predict response to these potent medicines.
On a personal note it was a great experience to undertake this research and I’m sure what I learned will hold me in good stead for research in the future. It was also highly beneficial to learn about a disease in depth that affects our community on such a significant scale. I would like to thank Warner and Patsy Mauger for their very generous
sponsorship through the Bowel and Liver Trust: this would not have been possible without their help.
Tom CurrieRead More...Other completed projects

Many other projects have been completed of which some are listed below
- IBD Database funding
- The cost and Disability of Ileal Pouch- Anal stenosis
- Chron’s and Colitis Support group grant
- Summer Studentship
- James Falvey NZSC Fellowship
- S100A12 Neutrophil Profile analysis
- CTV Colonoscopy
- Hepatitis Nurse Salary
- Salary IBD nurse
- Enteric pathogen testing
- James Falvey PhD project
- The costs of IBD summer studentship research
- Determinents of Intestinal failure
- Establishment of Liver Disease Database
- Association of PHOX2B, NCF4, FAM92B genes with IBD

